June 20, 2022
Curing the World by Changing It: Remembering Paul Farmer
By Adia Benton
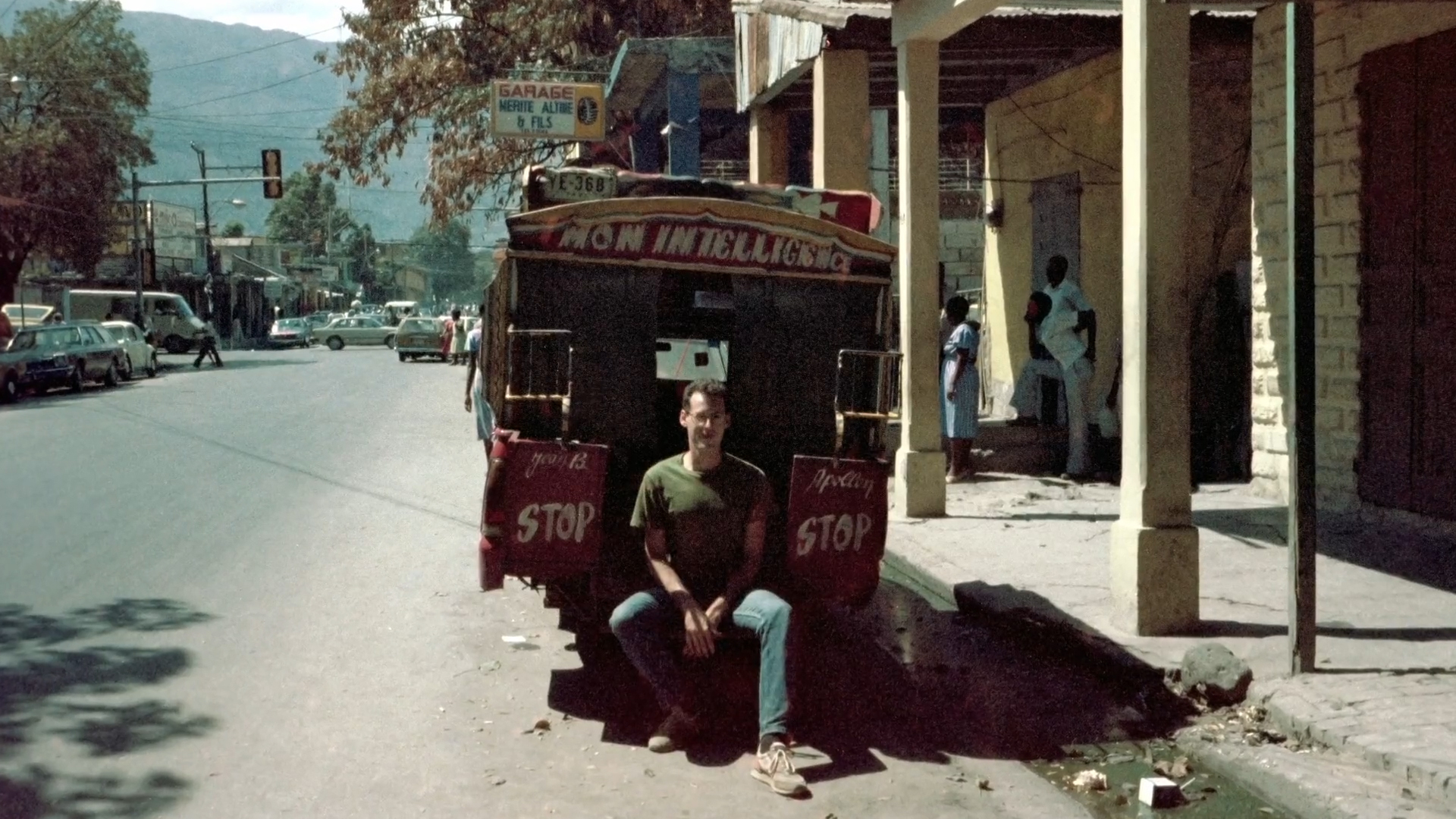
In the days after his death on February 21, 2022, Paul Farmer was most poignantly remembered as a clinician, public health expert, and humanitarian hero. The remembrances chronicled his significant contributions to global health as an “equity” evangelist—the genesis of which had been described, to some extent, solidified in collective consciousness in Tracy Kidder’s biographical account, Mountains Beyond Mountains: The Quest of Dr. Paul Farmer, A Man Who Would Cure the World. For many, Kidder’s book was the only entry into Paul Farmer’s life’s work, offering an origin story to match the outsized impact Farmer—along with his colleagues at Partners in Health and around the world—would have in shaping global health institutions, ideology, and practice. (I admit to having only read a part of it during my father’s convalescence in hospice care in late summer 2021. As my father was dying, Paul sent comforting words about his own father’s sudden death from a heart attack at the age of 49. I hadn’t read the book before, because it seemed weird to read a biography of a living, breathing friend and colleague with whom I regularly communicated). A former collaborator of mine, who was mentored and supervised by Paul in the 2010s, wondered in an email after his death, if his experience with Paul might have been different if they had met before the book was published. Before the legend was written.
Judging by those published remembrances online, even the most personal of them seemed to communicate that the most salient legacy of Farmer’s work was on “equity”—a buzzword now tacked on to “global health,” which prioritizes “fairness” in the practice and priorities of the practice of public health on a global scale. For many in global health, this has often translated into prevention and low-cost, low-tech solutions for health provided by entities located in rich countries, to people living in low- and middle-income countries—countries that are often also referred to as “Third World” or “The Global South.” But for Paul, this meant delivering the best quality health care everywhere, as a central component of progressing the social, economic, and human rights of the poor. Despite protests by some of his liberal interlocutors in the academy, he and his colleagues deliberately used “the poor” as a way of making common cause with people and communities “subordinat[e] within a global economic network that has limited [their] choices.”1 In Pathologies of Power, he “underlined the pathogenic role of inequity,” arguing that the “calls of a right to equity must necessarily contend with steep grades of inequality across as well as within international borders.”2 In focusing on the pathogenic role of inequity, he and his colleagues insisted that we contend with how capitalism, and the unfettered growth, expropriation, and immiseration that it entails, made people sick and exposed them to premature death; relatedly, the clinician who sought common cause with the “destitute sick,” would need to contend not only with individual patients’ maladies but also with the economic circumstances shaping their existence.
I first met Paul in 1997, I think, when I was an undergraduate at Brown, and he was invited to a class I would later teach at the same university fifteen years later: AIDS in International Perspective. He was friends with the course instructors, two women born in the 1930s who were also pioneers in medical anthropology and reproductive justice. One of them, Pat Symonds, had supported Partners in Health and worked at the Institute for Health and Social Justice (IHSJ) that Paul helped set up as the research, education, and advocacy arm of Partners in Health with his MacArthur Foundation Fellowship. The Institute hosted fellowships and seminars at Harvard’s medical and public health schools, which revolved “around the concept of scholars in service to the community.” A 1995 fellowship recruitment ad for the IHSJ, for example, emphasized that “fellows will receive unique training in both analysis—by exploring from the perspective of poor communities the health impact of developmental ‘aid’ programs, and how those programs come to be established; and practice—by working with a community-based organization that serves the poor.”3 The IHSJ also published several edited volumes focused on the themes of each fellowship year.
“Doctor, when all around you, liars are the only cocks crowing, telling the truth is a victory.”
The course, AIDS in International Perspective, was tough: we studied and discussed hundreds of pages of reading per week, hosted AIDS activists and researchers, and embarked upon projects with AIDS community service organizations in Rhode Island. The week before Paul’s visit to our class, our professors had only told us that the author of our assigned reading would be visiting and that he was “adorable.” (A cynical teenager who had better things to do, I probably rolled my eyes at the description. One of my classmates, Ian, chuckled as he parroted an enthusiastic statement by one of the professors, “And he has a Haitian wife!”). This “adorable” anthropologist and physician, at the time in his late 30s, had already written and published two books, and co-edited a third, by the time we hosted him in our classroom. We had to read two of those three books for seminar: AIDS and Accusation: Haiti and the Geography of Blame and Women, Poverty and AIDS: Sex, Drugs and Structural Violence (co-edited with Janie Simmons and Margaret Connors for the IHSJ). I had prioritized studying for my immunology and genetics mid-term exams, so I had barely touched the books by the time I arrived in class to await our guest.
When I entered the classroom that day, our usually small and intimate seminar of nine or ten students had grown by four or five students. (I would later learn that those extra students in attendance were of Haitian heritage and were already acquainted with his pioneering work). During his lecture, Paul discussed Women, Poverty and AIDS, which would serve as a manual of sorts as I carried out community work in AIDS service organizations over the coming years. What he and his co-authors and editors did in the book, awakened a critical sensibility for epidemiological, social science, and public health literatures in many of us. The book was prompted by inattention to patriarchy and gender, capitalism and class, racialization and racism, in the social science, public health, and clinical literature on HIV/AIDS. Paul and his colleagues, following feminist sociologist Patricia Hill-Collins, foregrounded an intersectional analysis; in so doing, they found victim-blaming and the inflation “of personal choice (or cultural difference)”—what he called “immodest claims of causality” elsewhere—lying at the root of many research, clinical, and social service programs for HIV prevention and care.4
A fundamental aim of the book, then, was not only to redress this by writing about and from the perspectives of poor women affected by the disease, but to also “re-read” and “re-think” the scholarly literatures critically, with care for poor women at the center of these critical re-readings. In part, this also meant incorporating poor women’s perspectives and their own astute political analyses of the conditions in their communities. A chapter in Women, Poverty and AIDS features a story of a group of self-described malarez (poor) Haitian women who, in light of high rates of HIV transmission, developed an education program during which they showed a video they made, demonstrated proper condom use, and facilitated community discussions. When they presented their work at a conference in Haiti, a doctor in the audience asked, “So what? In other words, if we are manifestly failing to prevent HIV transmission in this region, what is the significance of your project?” A woman from the group responded, “Doctor, when all around you, liars are the only cocks crowing, telling the truth is a victory.”5
Hewing closely to the lesson offered by this malarez, Paul outlined a few key points for addressing HIV/AIDS: telling the “truth” about the transmission dynamics among poor women, which would include examining sexism, racism, and classism together as risk factors for HIV/AIDS; education for preventing HIV/AIDS would be insufficient if it did not also address sexism and sexuality, universally; protecting, rather than punishing sex workers, as we work to address poverty, gender inequality and racism; improving clinical care by also improving the knowledge of clinicians about women and AIDS (at the time of his writing, HIV infection was under-recognized in women). The chapter foreshadows and alludes, too, to the third portion of the book, which highlights the work of organizations engaging in direct action to provide comprehensive care for HIV-positive and at-risk women, via housing, employment, and health services.
As Paul spoke to the class, I found myself flipping through the two books, furiously seeking out passages that aligned with what he was saying. I approached him after class. “What do you want?” he asked, conspiratorially, as if he had seen evidence of the secret I thought I’d been hiding fairly well—that I had not completed the assignment. “I want to know more about multidrug resistant tuberculosis,” I stammered. “The social stuff you talked about.” It was probably a brief aside in the lecture, but the “social stuff” to which I alluded were common themes in his early body of work: understanding the social conditions that structured risk for disease and premature death (social epidemiology) and embedding personal experience in the larger social fields in which such experience takes on its meaning (cultural anthropology). It was compelling and exciting to me, and I’d hoped he could point me in the right direction. So he called his assistant over, who scribbled down my mailing address. Within a few days, I received a stack of photocopied journal articles in my campus mailbox.
I began writing in earnest about the treatment of tuberculosis patients in New York City, and later took up the topic for a global health course I took in my first year of public health school. Important insights from those papers, I would argue, set me on the course for thinking differently about epidemics, and what a critical social science—what Paul referred to as “resocializing disciplines”—might help me to do as a public health advocate and as a scholar. For my research and writing about HIV/AIDS care, support and treatment in Sierra Leone, as well as my research on Ebola in West Africa, it has meant unraveling the role of the humanitarian and development industries in shaping the health landscape there (rather than solely focusing on whether HIV-positive patients, a majority of them poor, posed “cultural barriers” to care), experiences of the poor accessing care and treatment, and the racialized character of epidemic response that prioritizes containment of disease, the protection of elites, and the circulation of capital and the accumulation of wealth over the provision of care.
These overlapping visions, one which saw oppressive structures like white supremacy, patriarchy, and capitalism as “sinful” and the other, which viewed capitalism as vampiric, deadening, and racializing, were implements in Paul’s intellectual toolkit.
A few years after my first meeting with Paul, I reached out to meet up at the 2000 American Public Health Association meeting held in Boston that year. He was slated to give a lecture in a ballroom. I saw some of my colleagues from public health school in the audience. I don’t even remember the topic; I recently tried, with little success, to locate the conference program and perhaps scour for a title or abstract. But I do remember that he received a standing ovation. I waited as Paul talked to everyone in a throng of admirers, raising my finger to let him know I’d arrived to chat. As the crowd cleared—his handlers probably had something to do with that clearing—Paul held my arm and told me to walk with him to a car that would be taking him to the airport. (This dynamic would persist well into our friendship—a call or text or walk or drive on the way to the airport). I complained that I was feeling alienated in my classes, that I had been hoping for some real critical engagement on political and economic issues. During class, my concerns were often met with hostility at worst, indifference at best. I was angry and hurt and wanted to give up on public health altogether. He told me, “I’m friends with so many people at your school who are interested in all of those things. You’re too young to be cynical. You can’t give up on making things better.” He gave me an email address, while goofily revealing that the others back in the ballroom had received his office address, but I had been given his personal email.
Within days of returning home to Atlanta, I emailed him, still despairing. And as he had done a few years before for my tuberculosis inquiry, he recommended some reading. This time, he said that he had been helped by having social theories that offered moral and ethical anchoring for his work. Liberation theology is where he’d found that guidance, that anchoring. He recommended two texts: Leonardo Boff and Clodovis Boff’s Introduction to Liberation Theology and Gustavo Gutierrez’s A Theology of Liberation. It also helped that a friend had also encouraged me to join Emory’s student association for Health and Human Rights; that colleague was also studying for a master’s in theology concurrently with public health, and had been part of Doctors for Global Health, a pioneering group working in liberation medicine, which they defined as, “the conscious, conscientious use of health to promote human dignity and social justice.” I had found a comrade in a place where I had felt adrift. The pieces began to fall together. During a conversation at Boston College’s School of Theology back in 2013, Paul explained the intellectual and spiritual debt to liberation theology’s preferential option for the poor, which refers to the tendency within Biblical texts to privilege living alongside and caring for the powerless, to the marginalized in a given society. He said:
In my scholarly work… liberation theologians have some very powerful ideas that could help us to understand, not only epidemics— … for people marginalized by social forces well beyond their control—it could help us to do medicine more effectively. Whether you’re talking about working in parts of Boston or [elsewhere] … I’ve never been to a place where the idea of a preferential option for the poor was not illuminating or useful.6
Again, it was a central idea not only for his clinical practice and advocacy, but in his role as an ethnographer among poor communities where he offered clinical care.
Paul would occasionally remind us that he had been an anthropologist for as long as he’d been a physician. “I am an anthropologist,” I heard him say at a meeting of the American Anthropological Association back in 2017, “any time I am awake.” His orientation toward the world, his clinical practice, his vision of public health, came from intensive study—of social theory, of human experience (and particularly illness experience and experiences of suffering), of liberation theology—and of growing up poor, of lapsed and then rekindled faith, in Florida. While it might be appealing to narrow his legacy to a desire to “cure the world,” as in the title of Kidder’s book—that is, practicing medicine on a global scale, with the aim of repairing the global body politic—Paul’s intellectual legacy and praxis extend beyond these. Among the important concepts from liberation theology guiding his work were an embodied practice of “accompaniment,” of “pragmatic solidarity” against structural violence, a phrasing he borrowed from peace studies scholar Johannes Galtung, to describe “the large-scale social and economic structures in which affliction is embedded.”7 In his attempts to further theorize and operationalize structural violence, Paul argued:
[The] concept of structural violence is intended to inform the study of the social machinery of oppression. Oppression is a result of many conditions, not the least of which reside in consciousness. We will therefore need to examine, as well, the roles played by the erasure of historical memory and other forms of desocialization as enabling conditions of structures that are both “sinful” and ostensibly “nobody’s fault.”
He of course faced some pushback among his anthropologist interlocutors and friends seeking more precise conceptual language for the various forms of violence experienced by the poor.
These insights from a theology of liberation, I think, would have had little heft, and gained little momentum if not for his coupling them with his training in critical medical anthropology with physician-anthropologist Arthur Kleinman, psychological anthropologist Byron Good, and medical sociologist Mary-Jo DelVecchio Good, and in legal anthropology and ethnographic method with Sally Falk Moore at Harvard, and his undergraduate education of the (Black) Marxist variety at Duke, and beyond. These overlapping visions, one which saw oppressive structures like white supremacy, patriarchy, and capitalism as “sinful” and the other, which viewed capitalism as vampiric, deadening, and racializing, were implements in Paul’s intellectual toolkit.
And these tools, along with those from clinical medicine, were only meaningful if they could be used to alleviate suffering. As he wrote in the book he co-authored with Gutierrez (a copy of which he had left in my office with an inscription and note):
…an understanding of poverty must be linked to efforts to end it. Father Gustavo has often noted, in his writing and in his speaking, that poverty means death. Nowhere is this more evident than in medicine; and most medical specialists and institutions are aware of the need to do something about it. Imagine trying to do clinical research in an American teaching hospital without providing any clinical services. The study of poverty without an expressed concern with ending it is seen with a hermeneutic of suspicion by most of the people with whom I’ve lived and worked. A preferential option for the poor informs our clinical work and also our efforts to move beyond individual patients to remedy inadequacies, inefficiencies, and gaps in health systems.8
—
Adia Benton is an anthropologist who teaches at Northwestern University. She is the author of HIV Exceptionalism: Development through Disease in Sierra Leone (University of Minnesota Press, 2015) and is currently writing a book about the 2014 West African Ebola outbreak.
Notes
- Paul Farmer, Margaret Connors, Janie Simmons, eds., Women, Poverty, and AIDS: Sex, Drugs, and Structural Violence (Monroe, ME: Common Courage Press, 1996), xix; emphasis in original.
- Paul Farmer, Pathologies of Power: Health, Human Rights, and the New War on the Poor (Berkeley, CA: University of California Press, 2005), 20.
- Kristin Nelson, “Fellowship Health Social Justice,” Anthropology newsgroups mailing list archives, February 17, 1995, https://unauthorised.org/anthropology/sci.anthropology/february-1995/0630.html.
- Farmer, Connors, and Simmons, eds., Women, Poverty, and AIDS, 33.
- Farmer, Connors, and Simmons, eds., Women, Poverty, and AIDS, 34.
- Paul Farmer (in conversation with Roberto Goizueta), “Accompaniment: Liberation Theology, Solidarity, and a Life of Service,” Boston College School of Theology and Ministry Continuing Education, Jun 12, 2018, YouTube video, 1:16:03, https://youtu.be/hyfIAc2bW7o.
- Paul Farmer, “An Anthropology of Structural Violence,” Current Anthropology 45, no. 3 (June 2004): 305–325, https://www.jstor.org/stable/10.1086/382250.
- Jennie Weiss Block and Michael Patrick Griffin, eds., In the Company of the Poor: Conversations with Dr. Paul Farmer and Fr. Gustavo Gutierrez (Ossining, NY: Orbis Books, 2013).